In May, Dr. Rayzel Shulman and her team published the KiT Protocol in BMJ Open. This protocol is another step towards successfully moving forward the Keeping in Touch (KiT) program, which aims to support youth as they transition to adult type 1 diabetes care.
The transition from pediatric to adult care is one of the most fraught in the type 1 diabetes journey. As children, those with type 1 often have their health care supported and managed by their parents, and they have typically grown comfortable with their medical providers and team over many years.
At 18, when they must transition to adult care, they are often managing a host of other transitions—the start of post-secondary education, leaving home for the first time, managing first jobs or first romances. An enormous change to their healthcare team may result in a disconnect that leads to missed appointments, disinterest in diabetes management, and even a decision to simply stop receiving regular care.
All of this can lead to poor health outcomes, which is why researchers have been investigating ways to make these transitions easier for everyone. The idea to use digital solutions to improve the experience led to the development of KiT.
A multisite, randomised control trial, KiT is being run in four pediatric diabetes clinics in Ontario and two in Quebec. Co-PI, Dr. Meranda Nakhla, a pediatric endocrinologist at the Montreal Children’s Hospital, is leading the study in Quebec. KiT uses text-message-based communication to encourage education, follow up and care. Shulman, a pediatric endocrinologist at The Hospital for Sick Children (SickKids) in Toronto, notes that text messaging is an effective way to engage with adolescents and young adults. “This population is very invested in texting,” she explains, noting that it reduces many of the barriers to communication that come when leaving voice messages or asking someone to use an app.
Working with co-PI, Dr. Joseph Cafazzo, at the Centre for Digital Therapeutics at UHN, and Memotext, a platform for co-creation of digital patient engagement, Shulman and her team developed the program. Research participants are recruited within four months of their last pediatric visit. They are then randomized into a group with either no intervention or one where they are using KiT.
The group using KiT is provided with a personalized education program developed using online transition resources identified by co-PI, Dr. Anne-Sophie Brazeau. Participants receive regular text messages about topics related to transition to adult care based on data collected from the Readiness of Emerging Adults with Diabetes Diagnosed in Youth (READDY) tool. This enables the participants to receive support in identified areas they need most. KiT also gives an option for the participants to receive support in topics that are of interest to them. Patient Partners, including lead partner Marley Greenberg, helped to ensure the messages were relevant, as well as written appropriately for the age group they were meant to serve. “The text messages have a youthful flavour,” Shulman notes, “There are lots of emojis, but they also contain links to trusted sources of information.”
Alongside messages with useful tips, KiT helps coordinate ongoing diabetes care. Scheduled texts come in to check if the final pediatric visit has been booked, and if the new adult appointment is scheduled. It also provides reminders about upcoming scheduled follow-up visits. Shulman notes that this isn’t just an appointment reminder, but much more in-depth: asking participants if they have completed any required labs before their visit, uploaded data from their pump and/or sensor, if they have registered for a patient portal (if one exists at their clinic), and provides other specific information such as contact information for the adult endocrinology clinic they will be attending. KiT can explain what to expect at the clinic, as well as allow you to jot down notes or questions that it can remind you about before your scheduled appointment.
And if the participant has questions throughout the year? KiT is set up to recognize keywords, like hypoglycemia or alcohol, and send trusted information sources when the user texts a question that matches a keyword. This helps engage the young person and provide them with vetted resources to support their needs.
So far 57 young adults are participating in the study and the team is hoping to recruit a total of 210 within the next year. The team is also starting to study the implementation process. Co-PI, Dr. Laura Desveaux, an implementation scientist at Trillium Health Partners, will be assessing all data collected and interviewing participants to learn which components of KiT were used most and led to better outcomes and why.. This type of detailed assessment will help determine the next steps for the program as it develops and for understanding the final results of the KiT study.
Additionally, to determine the cost of adapting and implementing KiT, co-investigator Dr. Valeria Rac affiliated with University Health Network (UHN) and Diabetes Action Canada, is leading the cost of implementation analysis. This will help the team understand the costs associated with implementing and scaling KiT in a real-world clinical setting.
“The project as a whole is looking at self-efficacy as the main outcome and diabetes-related stigma and readiness to transition, and measures of glycemia as secondary outcomes,” says Shulman. “We hope that in the end this tool can help manage some of the gaps currently found in the process between pediatric and adult care, and support better long-term outcomes for young adults living with type 1 diabetes.”
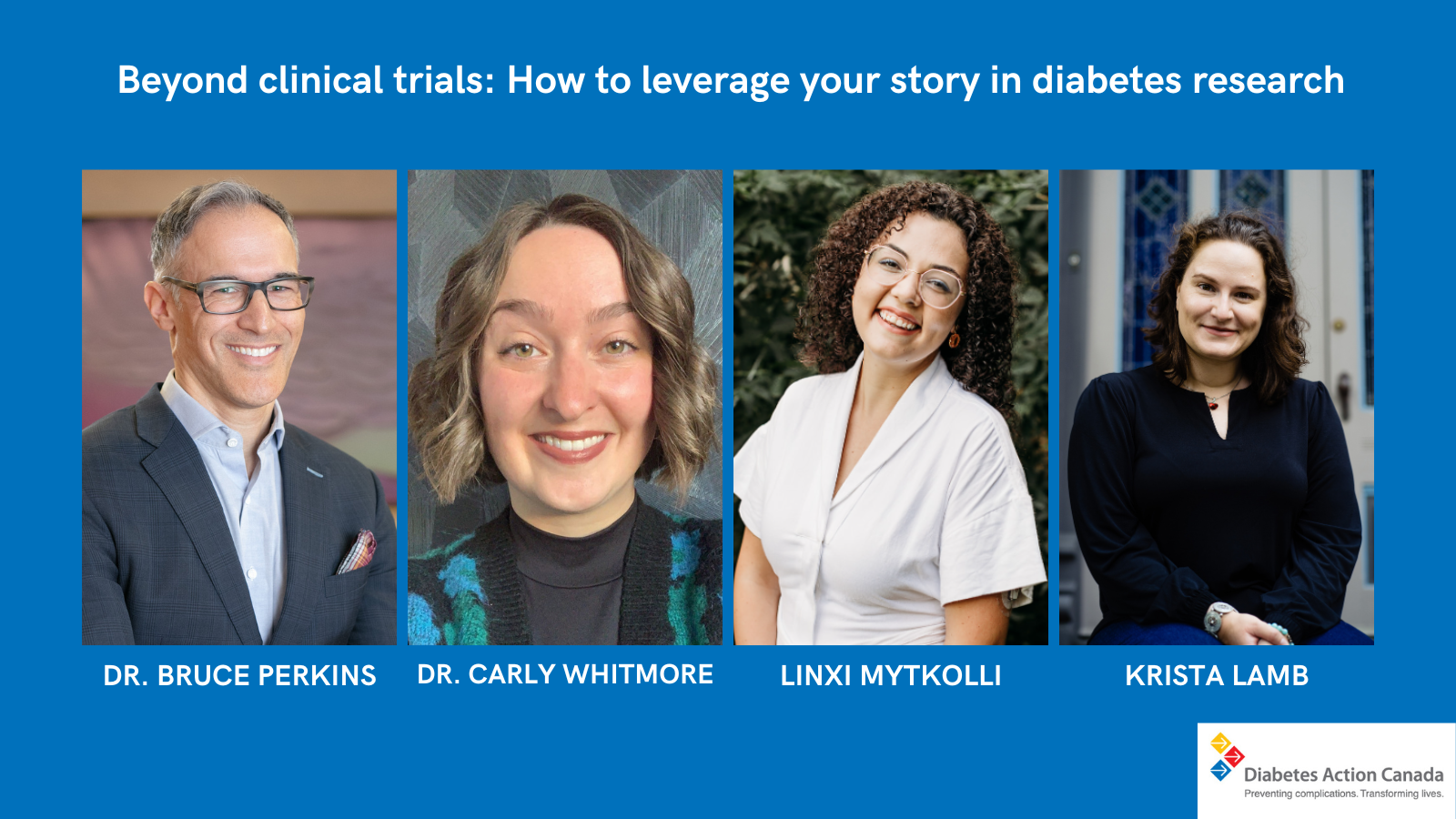
Written by Krista Lamb