Author: Krista Lamb
Second Edition of the Guidebook on Diabetes Management Out Now
The Banting and Best Diabetes Centre’s (BBDC’s) Knowledge Translation and Optimizing Care Models Program and Diabetes Pharmacists Network, recently released the second edition of their highly-regarded BBDC Guidebook on Diabetes Management.
Led by Dr. Lori MacCallum, a Diabetes Action Canada researcher, the latest edition incorporates recommendations from Canadian clinical practice guidelines in diabetes, hypertension, lipids and the use of antiplatelet agents. It also includes information health care providers need to know to help them implement these recommendations, including detailed information on over 100 medications, clinical pearls, helpful tips for educating patients using motivational interviewing techniques and for managing common side effects.
To order your copy, visit the U of T Bookstore.
New study from Diabetes Action Canada researcher highlights increase in diabetes-related amputation in Ontario
Recently, a study led by Diabetes Action Canada researcher Charles de Mestral from St. Michael’s Hospital in Toronto was released in CMAJ.
This study shows lower-limb amputation rates for those with diabetes in Ontario are rising, which highlights the need for improvements in care and access to resources in order to slow this progression.
“This study makes clear that healthcare professionals and policy makers need to work together to uncover the root causes of this increase and develop solutions to improve outcomes for people living with diabetes,” says Dr. Gary Lewis, Scientific Co-Lead for Diabetes Action Canada. “While this rise may seem small when compared against the overall increase in type 2 diabetes diagnosis in the province, it hammers home the need to be vigilant about foot care. Amputation is one of the most dreaded potential consequences of diabetes and it is critical we continue to advocate for improved outcomes in this area.”
While this study does not provide a clear reason for why this increase is occurring, it does remind us that there are things clinicians and patients can do to help in lowering the risk of a diabetes-related amputation.
Dr. Bruce Perkins’ provides a commentary in the same issue of CMAJ, which looks at some of the important takeaways for clinicians from this study. This includes renewed efforts to understand the underlying causes for this rise and to improve on the processes for identifying those at risk and improving preventive care.
For those with diabetes, this study is a reminder of the need to be vigilant about foot care. Amputation is a scary potential complication. However, there are things a patient can do to help decrease the risk:
- If you have diabetes, check your feet daily – contact your healthcare professional right away if you see any cuts, sores or signs of infection.
- If you have diabetes, it’s critical to get your feet checked regularly by a health care provider.
- If your doctor or endocrinologist does not suggest a foot assessment, don’t fear asking them for a referral.
- If foot care is difficult to access in your community, ask your health care provider to help you find the resources you need.
Diabetes Canada offers a helpful checklist for those with diabetes to help support better foot care. You can access it on their website.
For more information about the work Diabetes Action Canada is doing in this area, visit the section of our website on Foot Care and Prevention of Amputation.
Supporting diabetes patients with complex conditions (Ontario SPOR SUPPORT Unit Newsletter)
How is diabetes managed in the frail elderly? Read how OSSU, Better Access and Care for Complex Needs (BeACCoN) and Diabetes Action Canada address these complex health conditions in a complex health system, a first-of-its-kind collaboration. The full story can be seen in OSSU’s newsletter. Click Here to read full story
 Diabetes Action Canada will like to congratulate Dr. Michelle Greiver on being awarded a $2.6 million competitive operating grant. The grant will fund a SPIDER (Structured Process Informed by Data, Evidence and Research) approach, supporting primary care practices in optimizing care for patients with complex needs.
Diabetes Action Canada will like to congratulate Dr. Michelle Greiver on being awarded a $2.6 million competitive operating grant. The grant will fund a SPIDER (Structured Process Informed by Data, Evidence and Research) approach, supporting primary care practices in optimizing care for patients with complex needs.
CLick here to read the full article published by Canadian Health Care Technology
Dépistage de la rétinopathie diabétique
Dépistage de la rétinopathie diabétique
Responsables
- Michael Brent
- David Maberley
- Olivera Sutakovic
Chercheurs associés : Marie Carole Boucher, Melanie Campbell, Varun Chaudhary, Alan Cruess, Sherif El Defrawy, Mahyar Etminan, Bernard Hurley, Stephen Kosar, Jason Noble, Chris Rudnisky, Tom Sheidow, David Wong
Objectifs
Prévenir la cécité grâce au programme de dépistage rétinien à distance
Déterminer le rapport coût-efficacité associé au programme de dépistage rétinien à distance
Consulter les personnes diabétiques pour comprendre, selon le point de vue des populations vulnérables, les facteurs qui freinent ou facilitent l’accès au dépistage de la rétinopathie diabétique
Répertorier et faire participer les personnes qui sont à risque de développer une rétinopathie diabétique pour entamer le dépistage préventif
Utiliser l’intelligence artificielle et l’apprentissage machine (lecture automatique des images de la rétine) pour détecter la rétinopathie diabétique et d’autres maladies des yeux
Les personnes diabétiques sont plus à risque d’être aux prises avec un trouble de la vision. L’excès chronique de sucre dans le sang peut endommager le fond de l’œil (rétine), entraînant une enflure, des saignements et des cicatrices; il peut en résulter un trouble de la vision, voire une perte de la vue. Maladie qui peut rendre aveugle, la rétinopathie diabétique est une complication grave du diabète et constitue la principale cause de cécité chez les adultes de moins de 65 ans (en âge de travailler). Au stade précoce, la maladie ne présente aucun symptôme, mais elle peut rapidement évoluer aux stades avancés. Si elle n’est pas traitée, elle peut entraîner une grave perte de la vision et même la cécité.
Prévenir la cécité grâce au programme de dépistage rétinien à distance
Diabète Canada recommande à toutes les personnes diabétiques de se soumettre à un examen de la vue spécial chez un ophtalmologue ou un optométriste tous les ans ou tous les deux ans. Malgré cette recommandation, seulement 60 % des personnes diabétiques subissent régulièrement un examen de la vue. Pour cette raison, des milliers de Canadiens sont aux prises avec un trouble de la vision, l’une des complications du diabète parmi les plus redoutées.
La détection précoce de la rétinopathie diabétique, par un dépistage régulier de la rétine, est une méthode efficace pour prévenir la perte de la vision causée par le diabète. Il existe des traitements efficaces qui sont en mesure de prévenir la perte de la vision et de ralentir la progression des dommages s’ils sont détectés précocement. C’est pour cette raison qu’il est essentiel de soumettre toutes les personnes diabétiques à un examen de dépistage afin de détecter la présence de la rétinopathie diabétique à un stade précoce ou avancé.
Les jeunes adultes atteints du diabète de type 1, les Autochtones, les nouveaux immigrants et les personnes vivant dans les quartiers défavorisés des centres-villes et dans les collectivités éloignées affichent des taux de dépistage parmi les plus faibles. Malheureusement, nous savons que de nombreuses personnes diabétiques n’ont pas accès à des examens de la vue de manière régulière. Or, ces personnes ont la possibilité de subir un examen de la vue au moyen d’un système d’imagerie mobile (télémédecine), à savoir le programme de dépistage rétinien à distance. Les images de la rétine sont téléversées sur un serveur qui permet aux spécialistes de la rétine d’y accéder à distance. Ils peuvent ainsi évaluer l’état d’avancement de la rétinopathie, puis transmettre au fournisseur de soins primaires des recommandations relatives à la prise en charge de la maladie. À l’heure actuelle, plus de 500 sites offrent des services de dépistage de la rétinopathie diabétique à distance dans les quartiers défavorisés des centres-villes et dans les collectivités éloignées de l’Ontario, du Québec, de la Colombie-Britannique, de l’Alberta et du Manitoba; la majorité d’entre eux étant situés dans l’Ouest canadien. Toutefois, les programmes provinciaux n’étant pas uniformes, l’accessibilité au dépistage rétinien continue de poser problème.
Action diabète Canada s’efforce d’élaborer un programme national pour le dépistage rétinopathie diabétique qui visera à : prévenir les troubles de la vision et la cécité causés par le diabète; et éliminer les facteurs qui empêchent tous les Canadiens diabétiques d’avoir accès au service de dépistage. Notre groupe procède à la mise en œuvre d’une approche axée sur les pratiques exemplaires pour le diagnostic précoce et la prise en charge de la rétinopathie diabétique qui a de fortes chances d’être appliquée à grande échelle dans d’autres régions.
En Ontario, en partenariat avec Ontario Telehealth Network (OTN), Action diabète Canada envisage de collaborer avec chacun des réseaux locaux d’intégration des services de santé (RLISS) à la mise au point d’un programme personnalisé et durable qui pourra être intégré aux programmes régionaux de prise en charge des maladies chroniques déjà existants par l’entremise des centres de santé communautaires (CSC), des équipes de santé familiale, des programmes d’éducation sur le diabète et d’autres services. Le Dr Michael Brent, directeur national de notre groupe de travail sur le dépistage de la rétinopathie diabétique, a mis sur pied un programme de dépistage en collaboration avec des technologues experts dans les quartiers défavorisés des centres-villes et dans les collectivités éloignées présentant un nombre élevé de personnes diabétiques. Équipé d’un système portatif d’imagerie de la rétine, un technicien se rend d’un site à l’autre, fait subir au patient un examen de la vue pour le dépistage de la rétinopathie diabétique et lui transmet de l’information sur le diabète. Par la suite, les images de la rétine sont téléversées sur un serveur et rapidement évaluées par un ophtalmologue (le spécialiste de la rétine). Les personnes à risque ou qui ont besoin d’une intervention pour traiter une rétinopathie diabétique mettant en péril leur vue sont sans tarder renvoyées vers un spécialiste et prises en charge par les champions de la rétine de chaque RLISS.
Ce groupe a démontré la faisabilité et l’efficacité des mesures visant à diagnostiquer une maladie pouvant rendre aveugle qui était jusqu’alors passée inaperçue. Jugé prioritaire dans tous les RLISS de l’Ontario, ce programme est l’exemple parfait d’un projet qui vise à renforcer l’accès à des soins équitables, tout en illustrant le potentiel d’application à grande échelle du programme dans d’autres provinces et territoires. Par exemple, les responsables du programme de dépistage de la rétinopathie diabétique, dirigé par le Dr Stephen Kosar, en collaboration avec l’équipe de santé familiale du centre de santé de Manitoulin et l’OTN, axent présentement leur étude sur l’ensemble des personnes diabétiques d’origine autochtone vivant sur l’île Manitoulin.
En Colombie-Britannique, le Dr David Maberley, coresponsable de notre groupe de travail sur le dépistage de la rétinopathie, effectue actuellement une évaluation pragmatique de deux nouveaux sites de dépistage. Le premier est situé dans la communauté éloignée de la Première Nation Heiltsuk (Bella Bella); le deuxième, dans l’est du centre-ville de Vancouver. Ces sites serviront de base à l’élaboration d’un programme communautaire efficace pour le dépistage de la rétinopathie diabétique. À l’aide d’un nouveau logiciel pour la saisie de données sur les images de la rétine et la technologie de transfert, le groupe vise à automatiser l’analyse des images de manière à améliorer l’efficacité du programme de même que le triage des patients (à risque faible ou élevé) pour que l’équipe chargée des soins primaires ou spécialisés puisse leur offrir le traitement et le suivi appropriés.
Déterminer le rapport coût-efficacité associé au programme de dépistage rétinien à distance
Mme Valeria Rac (Toronto Health Economics and Technology Assessment ou THETA) a utilisé les données recueillies dans le cadre d’un projet pilote réalisé en collaboration avec le Centre de santé communautaire de Riverdale-Sud pour évaluer le rapport coût-efficacité associé au programme de dépistage rétinien à distance. Selon cette évaluation, ce programme, qui repose sur l’utilisation d’une caméra portative pour la prise d’images de la rétine, permet de détecter la rétinopathie diabétique à moindre coût, comparativement à l’examen de la vue courant effectué à des fins de dépistage dans les collectivités (semi)urbaines de Toronto auprès des personnes diabétiques qui sont à risque de développer cette maladie et qui n’ont pas accès aux spécialistes des soins de la vue.
Consulter les personnes diabétiques pour comprendre, selon le point de vue des populations vulnérables, les facteurs qui freinent ou facilitent l’accès au dépistage de la rétinopathie diabétique
En collaboration avec l’Université Laval et l’Institut de recherche de l’Hôpital d’Ottawa, nous avons mis sur pied un nouveau projet de recherche, pour lequel les responsables recrutent activement des participants en ce moment. À l’aide d’entrevues structurelles, l’équipe de projet vise à répertorier et à comprendre les facteurs qui freinent ou facilitent l’accès au dépistage de la rétinopathie diabétique en Ontario et au Québec chez les minorités ethnoculturelles qui courent un risque élevé de développer cette maladie (à savoir les immigrants originaires de l’Asie du Sud ou de la Chine ainsi que les immigrants francophones d’origine africaine). L’équipe de projet se servira des résultats obtenus pour mettre au point des interventions adaptées qui permettront concrètement d’éliminer les difficultés auxquels se heurtent ces groupes.
Répertorier et faire participer les personnes qui sont à risque de développer une rétinopathie diabétique pour entamer le dépistage préventif
Diabète Canada recommande à toutes les personnes diabétiques de se soumettre à un examen de la vue spécial chez un ophtalmologue ou un optométriste tous les ans ou tous les deux ans; les personnes présentant un risque élevé devraient, pour leur part, subir un examen plus fréquemment. Selon des données récentes, seulement 60 % des personnes diabétiques subissent un examen de la vue. Pour cette raison, des milliers de Canadiens sont aux prises avec un trouble de la vision. Nous envisageons d’utiliser les bases de données administratives provinciales et le Répertoire national du diabète pour répertorier les personnes diabétiques qui n’ont pas subi d’examen de la vue depuis plus de deux ans. Par la suite, nous avons l’intention d’entrer en contact avec ces personnes par l’entremise de leur centre de santé communautaire ou de leur professionnel en soins primaires afin de les inviter à un centre offrant des services de dépistage rétinien à distance pour les soumettre à un examen de dépistage de la rétinopathie diabétique. En communiquant directement avec ces patients, nous parviendrons à améliorer leurs connaissances au sujet de la rétinopathie diabétique, augmenter les taux de dépistage et prévenir la perte de la vision.
Utiliser l’intelligence artificielle et l’apprentissage machine (lecture automatique des images de la rétine) pour détecter la rétinopathie diabétique et d’autres maladies des yeux
La lecture des images de la rétine exige beaucoup de temps et demeure un processus essentiellement manuel. Au moment de la mise en œuvre à grande échelle du programme de dépistage rétinien à distance, nous serons confrontés à des obstacles majeurs en ce qui concerne le temps de lecture des images par les techniciens et les médecins. Nous espérons faire subir un examen de dépistage à tous les Canadiens qui sont à risque de développer la rétinopathie diabétique; or, la lecture des images sera une contrainte majeure qui risque de ralentir la pose du diagnostic et le début du traitement. Dans le cadre d’une nouvelle initiative stimulante réalisée en collaboration avec un groupe de chercheurs du Département d’ophtalmologie de l’Université de Montréal, de l’École polytechnique de Montréal et de l’Institut des algorithmes d’apprentissage de Montréal (MILA), Action diabète Canada étudie présentement le rôle que joue l’intelligence artificielle dans l’analyse des images de la rétine. Ce groupe de scientifiques procède à la mise au point de nouveaux algorithmes faisant appel à des technologies avancées pour faire la lecture des images du fond de la rétine et des images prises par tomographie par cohérence optique dans le but de poser un diagnostic de rétinopathie diabétique ou d’autres maladies oculaires. L’initiative axée sur l’intelligence artificielle permettra d’améliorer les soins et les résultats pour les personnes diabétiques, tout en facilitant l’accès aux spécialistes des soins de la vue et en augmentant la productivité des cliniciens.
Felfeli, R. Alon, R. Merritt et M.H. Brent. « Toronto tele-retinal screening program for the detection of diabetic retinopathy and macular edema in urban and rural settings: a case series », Journal canadien d’ophtalmologie, 2018. Consulté en ligne le 23 août 2018 : https://doi.org/10.1016/j.jcjo.2018.07.004.
Boucher, M. C., G. Desroches, R. Garcia-Salinas, A. Kherani, D. Maberley, S. Olivier et autres. « Teleophthalmology screening for diabetic retinopathy through mobile imaging units within Canada », Journal canadien d’ophtalmologie, 2008, 43(6), p. 658-668.
Hooper, P., M. C. Boucher, A. Cruess, K. G. Dawson, W. Delpero, M. Greve et autres. « Canadian Ophthalmological Society evidence-based clinical practice guidelines for the management of diabetic retinopathy », Journal canadien d’ophtalmologie, 2012, 47(2 Suppl):S1-30, S1-54.
Vieillissement, santé communautaire et des populations
vieillissement et la santé communautaire et des population
notre équipe
- Maureen Markle-Reid
- Jenny Ploeg
- Ruta Valatis
- Tracy Chmabers
Objectif
Travailler avec les aînés aux prises avec de multiples maladies chroniques et leurs proches aidants en vue de favoriser un vieillissement optimal à la maison
L’Unité de recherche sur la santé, la communauté et le vieillissement (URSCV) a récemment obtenu un financement grâce à une subvention des IRSC : Réseau de la SRAP sur les innovations en soins de santé de première ligne et intégré (ISSPLI) et à Action diabète Canada. Ce financement lui permettra de mener une étude à plusieurs sites intitulée programme de partenariat communautaire de l’URSCV visant à favoriser l’autoprise en charge du diabète chez les aînés canadiens.
Contexte : Adopté par l’Unité de recherche sur la santé, la communauté et le vieillissement (URSCV), le programme de partenariat communautaire est une intervention de six mois qui vise à favoriser l’autoprise en charge du diabète chez les aînés diabétiques qui sont aux prises avec d’autres maladies chroniques et à offrir du soutien à leurs proches aidants (famille ou amis). Il vise à améliorer les résultats associés à l’objectif à quatre visées : 1) la santé des populations; 2) l’expérience des patients et des proches aidants; 3) l’expérience des fournisseurs de soins; et 4) les coûts. Le programme de recherche s’appuie sur les données probantes faisant état de la faisabilité et de l’efficacité du programme de partenariat communautaire de l’URSCV qui ont été recueillies dans le cadre de nos travaux antérieurs. Il a été conçu dans l’optique de le mettre en œuvre à grande l’échelle.
Objectif de l’étude : L’approche consiste en une intervention de six mois qui s’articule autour de plusieurs volets et qui repose sur des données probantes. Elle a pour objectif d’intégrer les soins dans tous les milieux de manière à améliorer la qualité des soins et les résultats en matière de santé pour les aînés diabétiques (65 ans ou plus) qui vivent dans la collectivité et qui sont aux prises avec au moins une autre maladie concomitante, et à offrir du soutien à leurs proches aidants (famille ou amis).
Cette intervention s’articule autour de quatre volets principaux qui mettent à profit l’expertise des fournisseurs de soins de santé œuvrant dans des disciplines différentes. Elle prévoit également la mise en place d’un partenariat entre les organismes communautaires spécialisés en soins primaires :
Coordination des soins et navigation dans le système sous la direction d’une infirmière;
Visites à domicile réalisées par des éducateurs agréés en diabète (infirmières autorisées et diététistes) œuvrant pour les programmes d’éducation sur le diabète en lien avec les soins primaires;
Séances de groupe communautaires mensuelles animées conjointement par un partenaire communautaire (p. ex., YMCA) et un représentant du programme d’éducation sur le diabète associé aux soins primaires;
Conférences de cas mensuelles pour l’équipe d’intervention.
Des études ont démontré que, d’un point de vue statistique, la qualité de vie, notamment la santé mentale, et l’autoprise en charge de la maladie chez les aînés qui bénéficiaient du programme de partenariat communautaire de l’URSCV en Ontario s’étaient considérablement améliorées, en comparaison aux patients qui recevaient les soins habituels pour le diabète. De plus, leurs symptômes de dépression s’étaient mieux résorbés. L’intervention a été bien accueillie par les patients, les aidants et les fournisseurs de services. Qui plus est, les améliorations décrites ont été réalisées sans engendrer de frais supplémentaires pour l’ensemble du système de santé. Enfin, des données préliminaires portent à croire que le programme de l’URSCV, une fois mis en œuvre à grande échelle, procurera des bienfaits et permettra de réaliser des économies.
Des études ont démontré que, d’un point de vue statistique, la qualité de vie, notamment la santé mentale, et l’autoprise en charge de la maladie chez les aînés qui bénéficiaient du programme de partenariat communautaire de l’URSCV en Ontario s’étaient considérablement améliorées, en comparaison aux patients qui recevaient les soins habituels pour le diabète. De plus, leurs symptômes de dépression s’étaient mieux résorbés. L’intervention a été bien accueillie par les patients, les aidants et les fournisseurs de services. Qui plus est, les améliorations décrites ont été réalisées sans engendrer de frais supplémentaires pour l’ensemble du système de santé. Enfin, des données préliminaires portent à croire que le programme de l’URSCV, une fois mis en œuvre à grande échelle, procurera des bienfaits et permettra de réaliser des économies.
Effets sur le système de santé et les patients
Des soins axés sur la personne pour les patients ayant des besoins élevés/faisant grand usage du système de soins
La mise en œuvre de l’intervention auprès des populations diversifiées de l’Ontario, du Québec et de l’Île-du-Prince-Édouard, où les participants sont délibérément choisis parmi certaines des populations les plus vulnérables, permettra de cerner avec exactitude les pratiques exemplaires ou inefficaces et de comprendre les raisons de cette situation. De cette manière, l’équipe de recherche pourra recueillir l’information nécessaire pour restructurer les programmes en place pour la prise en charge du diabète et des maladies chroniques, lesquels doivent être personnalisés pour répondre aux besoins propres à chaque population.
Modèle général relatif à la mise en œuvre à grande échelle des interventions en faveur de l’atteinte de résultats dans toute la province
En plus de produire des données probantes visant à élargir la portée du programme de partenariat communautaire de l’URSCV, le programme permettra de mettre à l’essai un modèle général relatif à la « mise en œuvre à grande échelle » des interventions. En collaboration avec les responsables du programme d’application des connaissances d’Action diabète Canada, l’équipe de recherche étudiera la possibilité d’appliquer ce programme à grande échelle et cherchera de nouveaux sites destinés à sa mise en œuvre. Les résultats obtenus feront progresser la science liée à la mise en œuvre en fournissant de l’information concrète sur les étapes, les processus, les rôles et les responsabilités nécessaires pour implanter à grande échelle en Ontario, au Québec et à l’Île-du-Prince-Édouard une intervention prometteuse qui a fait ses preuves dans un environnement de recherche. La collaboration entre les chercheurs, les patients, le ministère, les fournisseurs de services de santé et les partenaires communautaires permettra de perfectionner et mettre au point de manière concertée le plan relatif à la mise en œuvre à grande échelle. Grâce à cette approche, il sera possible de répondre aux besoins de tous les intervenants qui participeront au financement, à la prestation des services ou à leur réception.
Renforcer les capacités afin de favoriser un système de santé axé sur l’apprentissage intersectoriel
Cette étude a pour but d’aider les intervenants œuvrant dans des secteurs différents à apprendre les uns des autres. La mise en œuvre de l’intervention favorise la collaboration, car elle donne aux divers fournisseurs de services la possibilité de communiquer régulièrement et de bénéficier de séances de formation commune. Grâce à cette approche, ils sont en mesure d’apprendre les uns des autres et de comprendre à quel point les autres secteurs contribuent à améliorer les soins axés sur la personne.
Engagement des patients
Under construction
Application des connaissances (AC)
Under construction
Innovations liées au diabète de type 1
Under construction
Santé des peuples autochtones
Under Constrcution
Évaluation des technologies de la santé et du réseau
Under construction
Soins des pieds pour prévenir les amputations des membres inférieurs
Under construction
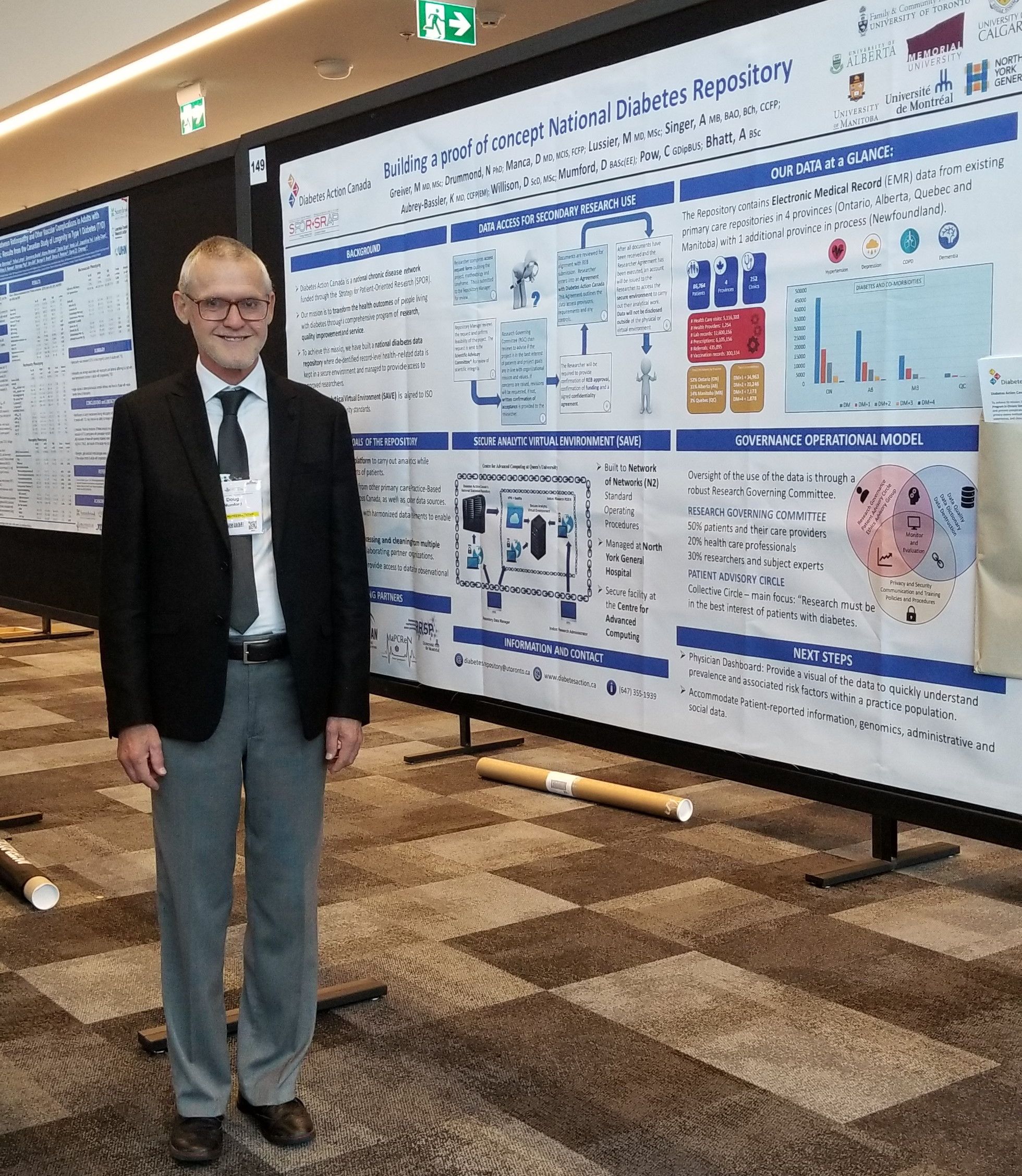
Diabetes Research Gets a Security Upgrade
The National Diabetes Repository is making great strides in transforming health outcomes for Canadians. The National Diabetes Repository is a secure research environment in which researchers can run advanced analysis on health data-sets to study behaviour trends and how to better treat people with diabetes to prevent complications. In a recent article by Compute Ontario, Conrad Pow, our Senior Project Manager for the National Diabetes Repository comments on the utility of the digital tool and how it can accelerate research studies using health data in diabetes. To read more about this article and partnership with Compute Ontario please read the full article here
OSSU CMAJ Supplement RELEASED- Engaging Patients in Health Research
Message from the Ontario SPOR SUPPORT UNIT (OSSU)
OSSU is pleased to share with you a special supplement highlighting the value of patient engagement in research through 17 innovative OSSU-funded IMPACT Demonstration projects. Engaging Patients in Health Research: the Ontario Experience, published today in CMAJ (Canadian Medical Association Journal), features in-the-trenches experiences, tips and challenges from 17 IMPACT projects ranging from youth involvement in mental health services to suicide prevention, Indigenous health, children with complex medical needs and more.
The comprehensive collection of articles is a resource for researchers and others interested in this growing approach that involves patients and caregivers as partners in health and health systems research. It is also a valuable addition to the literature.
An infographic and an engaging podcast featuring interviews with researchers and patients provide excellent overviews of the content.
As a stakeholder in patient-oriented research, we thought you would be interested in this unique collection. Please feel free to share it through your networks, on social media and through other communications channels.
Vasanthi Srinivasan
CNIB Eye Van truck-trailer to be replaced for 2019 tour
SUDBURY—The CNIB (Canadian National Institute for the Blind) Medical Mobile Care Unit will once again serve around 4,500 patients on its annual tour of Northern Ontario. However, this will be the last time the present unit will make the trip, as a new unit will be in place for next year’s tour.
Click Here to read full story as published by Tom Sasvari on the Manitoulin Expositor
Congratulations Dr. Michelle Griever, the new Gordon F. Cheesbrough Research Chair
 Diabetes Action Canada will like to congratulate Dr. Michelle Greiver on her appointment as the new Gordon F. Cheesbrough Research Chair in Family and Community Medicine at North York General Hospital (NYGH) and Director of the University of Toronto Practice-Based Research Network (UTOPIAN) at the Department of Family and Community Medicine (DFCM)
Diabetes Action Canada will like to congratulate Dr. Michelle Greiver on her appointment as the new Gordon F. Cheesbrough Research Chair in Family and Community Medicine at North York General Hospital (NYGH) and Director of the University of Toronto Practice-Based Research Network (UTOPIAN) at the Department of Family and Community Medicine (DFCM)
Dr. Greiver comes to the role after more than 15 years of experience with PBRNs. She was a founding member and then lead of the North Toronto Research Network (NorTReN). NorTReN was initiated under the leadership of past DFCM Chair Dr. Walter Rosser and was a precursor for UTOPIAN. Dr. Greiver then worked with Drs. Lynn Wilson, Eva Grunfeld and David White on the initial development and successful launch of UTOPIAN. She became Deputy Director of UTOPIAN in July 2016 and then Acting Director upon the departure of Dr. Frank Sullivan, inaugural Cheesbrough Chair and immediate past UTOPIAN Director, in April 2017.
Diabetes Action Canada is proud of you and your new endeavor.
Click here to read full article as published by the Department of Family and Community Medicine University of Toronto.
Announcing the recipient of the Diabetes Action Canada Fellowship Awards 2018-2020
DAC Training and Mentorship Program Fellowship Awards 2018-2020
This year, the Diabetes Action Canada Training and Mentoring Program will be granting one Post-doctoral Fellowship Award, peer-reviewed by Diabetes Canada, of $50,000/year for a period of two years.
We are pleased to announce the successful recipient of the scholarship award for the Post-doctoral Fellowship 2018-2020:
Françoise Proust – Université de Laval, École de Nutrition
Congratulations Françoise and good luck with your research project!
Training and Mentoring Policies
Mentorship and Internship Procedural Plan
Application & Approval Process
- Information and application forms in both languages are provided on DAC website (follow-up with Cathy)
- Training & Mentoring Coordinator receives and screens application forms and relevant documents
- Training & Mentoring Coordinator adds applicants information to tracking database
- Training & Mentoring Goal Group Leads evaluate (using evaluation criteria/chart) and recommend to the Co-Scientific Leads
- Co-Scientific Leads submit the recommendations to the Steering Council (Quarterly meetings)
- Diabetes Action Canada Central Admin updates Training & Mentoring Coordinator on the decision of the Steering Council
Next Steps
Follow-up by Training & Mentoring Coordinator:
- informs awarded candidates and provides additional information if needed
- updates Mentorship/Internship tracking database
Mentorship/Internship Report reminders
- Training & Mentoring Coordinator monitors reminders for reports due
- Training & Mentoring Coordinator sends an email to candidates for reports
- Training & Mentoring Coordinator updates database
Award Selection Criteria
[bs_collapse id=”collapse_98de-f2a1″]
[bs_citem title=”
DAC TRAINING AND MENTORING APPLICATION REVIEW CRITERIA – MENTORSHIP PROGAM 2017-18
” id=”citem_f886-e674″ parent=”collapse_98de-f2a1″]
Eligibility criteria:
- The applicant must be a member of the DAC Network.
- Early career investigators must be within three years of their university appointment and have a research program deemed to be of excellent scientific quality. An appointment start date must be included in the Candidate’s Research Program Section of the application.
- The applicant’s research and mentorship plan must relate to diabetes and its complications.
- The applicant must propose a mentorship plan that demonstrates capacity building in Patient-Oriented Research (e.g. establishment of new multidisciplinary and/or intersectoral collaborations within a network of patient-oriented research).
- The applicant must have the support of 1) an internal mentor from his/her research centre, and 2) an external mentor from a different research centre recognized by CIHR. At least one of the two mentors should be a member of the DAC Network. These mentors should be actively involved in the scientific leadership of the applicant, including student co-supervision, scientific collaboration, access to specialized platforms, etc.
- The applicant must submit a mentorship plan that has been discussed and approved by both internal and external mentors. A detailed description of the mentorship plan should be submitted for evaluation.
- Submit a CIHR CCV (with the Detailed Contributions section) of the applicant and mentors (internal and external) to assess scientific excellence. If the mentors are outside Canada, any CV containing information similar to the CIHR CCV will be accepted.
- A one-year budget plan of expenditures (limit $10,000), see below for eligible expenses.
- Successful candidates agree to provide a brief report each year for 3 years to demonstrate the leverage effect of the program (i.e. new collaborations, obtaining scholarships and/or external grants).
Note: Although not a criterion, applicants from rural or less connected communities will be given priority if proposed research program deemed appropriate.The Diabetes Action Canada Network supports equity in its Mentorship program and encourages applications from qualified individuals, women or men, including Aboriginal people, persons with disabilities and members of visible minorities.
Application Evaluation Process:
- Potential of the candidate: Quality of research training, scientific achievements, history of publication, funding and training of students;
- Research program: Clarity of the research question and scientific justification. Potential for the creation of new knowledge, originality of assumptions and research questions, new approach, or methodologies or new application of existing methodologies;
- Affiliation and expertise of the proposed mentors;
- Relevance and quality of the proposed intercentre mentorship plan: Immediate or potential impact of mentorship for the early career investigator’s laboratory/research and research within the DAC Network (e.g. establishment of new multidisciplinary and/or intersectoral collaborations within a network of patient-oriented research);
- Feasibility of the proposed budget: Relevance of the proposed use of funds.
Scoring System – Scores out of 50
- QUALITY OF THE APPLICANT (TRAINING, PUBLICATIONS, ETC.) – 20 points
Applicant’s score: /20 points
- QUALITY OF THE MENTORSHIP PLAN AND ALIGNMENT WITH DIABETES ACTION CANADA NETWORK OBJECTIVES – 20 points
Applicant’s score: /20 points
- QUALITY OF THE MENTORS – 10 points
Applicant’s score: /10 points
Note: Considerations and pertinence related to POR (sex and gender, etc.) will be judged by the Patient Engagement Group in the next round.
[/bs_citem]
[bs_citem title=”
DAC TRAINING AND MENTORING APPLICATION REVIEW CRITERIA – INTERNSHIP PROGAM 2017-18
” id=”citem_93fc-939e” parent=”collapse_98de-f2a1″]
Eligibility criteria:
- The applicant must be a doctoral student, a postdoctoral fellow, a health professional research trainee, or a research professional and member of the DAC Network by the time of tenure of the grant (not necessarily before).
- The applicant’s supervisor must be a PI or Co-I of the DAC Network (e. before the application).
- Only one application per year per PI or Co-I in total may be submitted for this contest.
- Any applicant can only receive this support grant once.
- The applicant must provide a description of relevant training and integrate it into an intercentre collaborative project (incorporating at least two recognized research centers) involving at least one researcher of the DAC Network.
- Successful candidates agree to submit a scientific abstract for oral or poster presentation at the Annual Scientific Meeting of Diabetes Canada or other major national and international diabetes research conferences.
- Successful candidates agree to provide a brief progress report after the one-year funding and to respond to a short questionnaire yearly for another 2 years to document impact (i.e. new collaborations, obtaining scholarships and/or external grants).
Application Evaluation Criteria and Process:
For DAC PIs, Co-Is and collaborators:
- Excellence in home and host laboratories: Description of performance, scientific contribution and expertise of the laboratories involved in the collaboration;
- Relevance and quality of the proposed intercentre training: Immediate or potential impact of mentoring for the original laboratory and research within the network, according to its objectives (ex. establishment of new multidisciplinary and/or intersectoral collaborations inside the DAC Network or at an international level, knowledge transfer, patient-oriented research, standardization of methods, establishment of a platform or common resources, etc.);
- Feasibility of the proposed budget: Relevance of the proposed use of funds.
For the student/intern/resident/professional:
- For doctoral students, residents and postdoctoral fellows:
- Holding an excellent record of publication and participation/involvement in scientific activities.
- For research professionals:
- Must be actively involved in activities related to the priorities of the DAC Network as in research platforms, multi-centric projects, provincial, national or international research networks.
- Demonstrate motivation to pursue a career in research areas related to diabetes and its complications.
Note: Although not a criterion, applicants from rural or less connected communities will be given priority if proposed research project is deemed appropriate.
The Diabetes Action Canada Network supports equity in its Internship program and encourages applications from qualified individuals, women or men, including Aboriginal people, persons with disabilities and members of visible minorities.
Scoring System – Scores out of 50
- QUALITY OF THE APPLICANT (TRAINING, PUBLICATIONS, ETC.) – 20 points
Applicant’s score: /20 points
- QUALITY OF THE TRAINING PLAN AND ALIGNMENT WITH DIABETES ACTION CANADA NETWORK OBJECTIVES – 20 points
Applicant’s score: /20 points
- QUALITY OF THE MENTORS – 10 points
Applicant’s score: /10 points
Note: Considerations and pertinence related to POR (sex and gender, etc.) will be judged by the Patient Engagement Group in the next round.
[/bs_citem]
[bs_citem title=”
Patient-Oriented Research (POR) Early Career Investigator Mentorship Award in Diabetes and its Complications 2018-2019
” id=”citem_020f-d4cd” parent=”collapse_98de-f2a1″]
Diabetes Action Canada is launching its 2018-2019 Intercentre Mentorship award for early career investigators interested in Patient-Oriented Research (POR) in diabetes and its complications. The goal of this award is to promote networking and optimal integration of early career investigators into the Diabetes Action Canada (DAC) Network and the Canadian diabetes research community. Up to two (2) annual mentorship awards will be awarded to early career investigators to work with an internal mentor and an external mentor. The internal mentor will be affiliated to the same research centre as the early career investigator. The external mentor will be affiliated with a different research centre from that of the early career investigator. At least one mentor will be a regular member of the DAC Network. Mentors who are not PI’s or Co-I’s of DAC must become DAC members before the allocation of funds.
Eligibility criteria and methods of evaluation are described below. Successful candidates will receive financial support of a maximum of $10,000 for a one-year period to support their intercentre scientific activities.
Application deadline
The deadline for submission of applications is June 29th, 2018 for funding commencing no later than September1st, 2018.
Applications submitted late, incomplete or which do not meet the eligibility criteria will not be evaluated. Proposed mentoring must be completed within the year of holding the award.
If not a DAC Network member at the time of application, successful early career investigator applicants must apply to become members of the DAC Network before allocation of award funds. Successful applicants must complete a final report at the end of their mentorship year (December 2019) and agree to subsequent annual reports for an additional two (2) years to document the impact of this mentorship experience.
Eligibility criteria for the proposed candidate:
- The applicant must be a member of the DAC Network.
- Early career investigators must be within three years of their university appointment and have a research program deemed to be of excellent scientific quality. An appointment start date must be included in the Candidate’s Research Program Section of the application.
- The applicant’s research and mentorship plan must relate to diabetes and its complications.
- The applicant must propose a mentorship plan that demonstrates capacity building in patient-oriented research (e.g. establishment of new multidisciplinary and/or intersectoral collaborations within a network of patient-oriented research).
- The applicant must have the support of 1) an internal mentor from his/her research centre, and 2) an external mentor from a different research centre recognized by CIHR. At least one of the two mentors should be a member of the DAC Network. These mentors should be actively involved in the scientific leadership of the applicant, including student co-supervision, scientific collaboration, access to specialized platforms, etc.
- The applicant must submit a mentorship plan that has been discussed and approved by both internal and external mentors. A detailed description of the mentorship plan should be submitted for evaluation.
- Submit a CIHR CCV (with the Detailed Contributions section) of the applicant and mentors (internal and external) to assess scientific excellence. If the mentors are outside Canada, any CV containing information similar to the CIHR CCV will be accepted.
- A one-year budget plan of expenditures (limit $10,000), see below for eligible expenses.
- Successful candidates agree to provide a brief report each year for 3 years to demonstrate the leverage effect of the program (i.e. new collaborations, obtaining scholarships and/or external grants).
Note: Although not a criterion, applicants from rural or less connected communities will be given priority if proposed research program deemed appropriate.
The Diabetes Action Canada Network supports equity in its Mentorship program and encourages applications from qualified individuals, women or men, including Aboriginal people, persons with disabilities and members of visible minorities
Eligible Expenses:
Any expenses related to mentorship support for the recipient according to CIHR research grant standards. This may include:
- transportation and accommodation costs for external mentor visits to the early career investigator’s research centre;
- transportation and accommodation costs for the early career investigator to the external mentor’s research centre;
- transportation, accommodation and registration at conferences/meetings for the early career investigator if at least one of the mentors is present at the same event and a meeting is on the agenda; or
- costs related to intercentre scientific collaborations (support of early career investigators directly involved in the intercentre collaboration, supplies, technical services, etc.).
[/bs_citem]
[bs_citem title=”
Patient-Oriented Research (POR) Intercentre Trainee Internship Award in Diabetes and its Complications 2018-2019
” id=”citem_d129-44e0″ parent=”collapse_98de-f2a1″]
Diabetes Action Canada is launching its 2018-2019 Intercentre Internship competition for graduate students, postdoctoral fellows, and research professionals interested in Patient-Oriented Research (POR) in diabetes and its complications. The goal of this award is to promote networking and optimal integration of trainees into the Diabetes Action Canada (DAC) Network and the Canadian diabetes research community. Up to two (2) annual internships will be awarded to trainees. The DAC Network invites researchers who are PI’s or Co-I’s of the DAC Network to propose collaborative projects in the areas of diabetes and its complications and for which a trainee will complete his training in another laboratory (in another research centre). This project will involve a DAC Network PI or Co-I with one or more collaborators of another Patient-Oriented Research centre. Every collaborator must be a member of the DAC Network (or another SPOR Network) and participate in its activities.
Eligibility criteria and methods of evaluation are described below. Successful candidates will receive financial support of a maximum of $10,000 for a one-year period to allow the establishment of the trainee-based collaboration between the collaborators.
Application deadline
The deadline for submission of applications is June 29th, 2018 for funding commencing no later than September 1st, 2018.
Applications submitted late, incomplete or which do not meet the eligibility criteria will not be evaluated. Funded projects must be completed within the year of holding the award.
If not a DAC Network trainee member at the time of application, successful applicants must apply to become members of the DAC Network in order to receive the grant. Recipients must complete a final report at the end of their year of funding and agree to respond to subsequent annual short questionnaires for an additional two (2) years to document the impact of this internship experience.
Eligibility criteria:
- The applicant must be a doctoral student, a postdoctoral fellow, a health professional research trainee, or a research professional and member of the DAC Network by the time of tenure of the grant (not necessarily before).
- The applicant’s supervisor must be a PI or Co-I of the DAC Network (e. before the application).
- Only one application per year per PI or Co-I in total may be submitted for this contest
- Any applicant can only receive this support grant once.
- The applicant must provide a description of relevant training and integrate it into an intercentre collaborative project (incorporating at least two recognized research centres) involving at least one researcher of the DAC Network.
- Successful candidates agree to submit a scientific abstract for oral or poster presentation at the Annual Scientific Meeting of Diabetes Canada or other major national and international diabetes research conferences.
- Successful candidates agree to provide a brief progress report after the one-year funding and to respond to a short questionnaire yearly for another 2 years to document impact (i.e. new collaborations, obtaining scholarships and/or external grants).
Eligible Expenses:
Any expenses related to internship support for the recipient according to CIHR research grant standards. This may include:
- Transport, accommodation and living expenses (if necessary depending on the distance) for the trainee(s) in the collaboration laboratory;
- Shipping costs between the main laboratory and the collaboration laboratory(ies) in connection with the trainee’s stay;
- Purchase of supplies necessary for the trainee’s setup in the collaboration laboratory(ies) (the purchases can be made in the host laboratory or in the main laboratory).
Ineligible Expenses:
- Transport, accommodation and living expenses for the trainee in his/her main laboratory; Salary for trainees or other researchers.
Application Submission Process:
- Application form completed by the trainee or research personnel;
- A CIHR CCV (with the Detailed Contributions section) of the trainee or research personnel.
All documents must be submitted (in PDF format) to the DAC Training and Mentoring Coordinator, Michelle Murray, Michelle.Murray@umoncton.ca.
Application Evaluation Criteria and Process:
All applications will be assessed according to the eligibility criteria of the competition and the following criteria. Successful candidates will be notified by July 13th, 2018.
For DAC PI’s, Co-I’s and collaborators:
- Excellence in home and host laboratories: Description of performance, scientific contribution and expertise of the laboratories involved in the collaboration;
- Relevance and quality of the proposed intercentre training: Immediate or potential impact of mentoring for the original laboratory and research within the network, according to its objectives (ex. establishment of new multidisciplinary and/or intersectoral collaborations inside the DAC Network or at an international level, knowledge transfer, patient-oriented research, standardization of methods, establishment of a platform or common resources, etc.);
- Feasibility of the proposed budget: Relevance of the proposed use of funds.
For the student/intern/resident/professional:
- For doctoral students, residents and postdoctoral fellows:
- Holding an excellent record of publication and participation/involvement in scientific activities.
- For research professionals:
- Must be actively involved in activities related to the priorities of the DAC Network as in research platforms, multi-centric projects, provincial, national or international research networks.
- Demonstrate motivation to pursue a career in research areas related to diabetes and its complications.
Note: Although not a criterion, applicants from rural or less connected communities will be given priority if proposed research project is deemed appropriate.
The Diabetes Action Canada Network supports equity in its Internship program and encourages applications from qualified individuals, women or men, including Aboriginal people, persons with disabilities and members of visible minorities.
Any request for additional information can be forwarded to the DAC Training and Mentoring Coordinator, Michelle Murray, Michelle.Murray@umoncton.ca.
[/bs_citem]
[/bs_collapse]
Diabetes Action Canada Terms of Reference for Governance Committees
CONTENTS
[bs_collapse id=”collapse_dc4e-a604″]
[bs_citem title=”
1. Terms of Reference for the Steering Council
” id=”citem_658f-c555″ parent=”collapse_dc4e-a604″]
- Ensure that the Vision and Mission of the SPOR Network are fulfilled through a strategic, accountable, committed leadership and management functions
- Through the skill-based and partnership governance structure, create the highest quality oversight, communication, support and guidance for the conduct of the patient-oriented research goals using best (corporate) governance principles;
- Develop appropriate agreement and memorandum documents articulating terms suitable for membership in the SPOR Network including specific description of participation and co-investment of resource (time, expertise, infrastructure and revenues);
- Enable strict financial oversight using standard accounting and auditing measures;
- Promote strategic partnership relationships with inaugural (core) and new members (academic, public and private) of the SPOR Network with sensitivity to balancing gender, age, language (French, English);
- Incorporate local academic and clinical nodes of the Network in strategic project development, implementation and evaluation;
- Monitor governance performance including excellence and sustainability of the leadership, management and engagement of the participating members;
- Manage conflict of interest through appropriate processes including necessary agreements establish for all aspects of governance and research partnerships.
[/bs_citem]
[bs_citem title=”
2. Steering Council Executive
” id=”citem_375c-360e” parent=”collapse_dc4e-a604″]
- To review and approve the agendas for the Steering Council Meetings;
- To review strategic initiatives and partnership proposals brought forward by the Strategic Partnerships and Innovation Standing Committee;
- To review nomination of new members or re-appointment of members to the Steering Council and its Standing Committees, as proposed by the Nomination/Governance Standing Committee;
- To advise Co-Scientific leads and Executive Director about issues arising between meetings of the Steering Council that require executive decision;
- To review the draft Annual Financial Report to CIHR and Network Partners, as submitted by management with oversight by the Finance/Audit Standing Committee;
- To work closely with the Co-Scientific Leads and Executive Director on all matters related to fulfilling the objectives of Diabetes Action Canada.
[/bs_citem]
[bs_citem title=”
3. Standing Committees of the Steering Council
” id=”citem_9322-d7b5″ parent=”collapse_dc4e-a604″]
Members of the Steering Council along with other relevant leaders (e.g. Network Directors and collaborating experts) will serve on the following three Standing Committees:
- Strategic Partnerships and Innovation Standing Committee
- Nomination/Governance Standing Committee
- Finance/Audit Standing Committee
[/bs_citem]
[bs_citem title=”
4. Terms of Reference for the Standing Committees
” id=”citem_2abd-b60a” parent=”collapse_dc4e-a604″]
a) Strategic Partnerships and Innovation Standing Committee
- To develop and oversee the implementation of all the internal and external strategic partnerships for the collaborative research, KT and education projects that are undertaken by the Network Goal Groups;
- Responsible for advising about the ongoing strategic planning and evaluation of these activities;
- To receive the annual reports of each of the Goal Groups and the Scientific Advisory Panel and to advise the Steering Council;
- To advise about the strategic plans for support and sustainability of the Network.
b) Nomination/Governance Standing Committee
- To recruit and nominate members of the Steering Council including the Executive. A slate of new members will be brought forward to the Steering Council annually as necessary in their Fall Face-to-Face Meeting;
- The Committee Chair along with the Chair of the Steering Council and Co-Leads will be responsible for orientation of new members of the Council;
- Responsible for organizing and implementing the evaluation of the performance of the Steering Council as well as the annual performance of the Co-Leads (Academic);
- To assist in recruitment of Members of the Standing Committees of the Steering Council
c) Finance/Audit Standing Committee
- To develop the annual revenue/expense budget of the SPOR Network for approval by the Steering Council;
- To report the quarterly actual against budget to the Steering Council;
- To oversee the annual formal financial audit for the Network’s annual report.
- To recommend an auditor for the SPOR Network
[/bs_citem]
[bs_citem title=”
5. Patient-Oriented Research (POR) Program Committee
” id=”citem_a46d-7e0a” parent=”collapse_dc4e-a604″]
- Coordinates and monitors all research, KT and education translation activities within the Network with advice from the Patient Circles
- Ensure the work plans are executed with adherence to timelines
- Evaluative reporting on outputs and outcomes
- Advises the Steering Council about new Network members
- Provides guidance and feedback on strategic directions of the Network, including changes to implementation of projects or development of new opportunities
- Advises Goal Groups about new opportunities for acquiring new revenues and partners
- Receives annual reports of all of the projects and evaluates progress toward target deliverables and milestones
- Assists in preparation of the annual budget with the Executive Director and DAC Administrative team
- Assists the management team in ensuring timely reporting of the revenues and expenses and assessing financial targets according to the planned budget throughout the year
- Works closely with institutional fund-raising leads to leverage new resources to meet and exceed the target for matched funding
Members:
The POR Program Committee represents the core Principal Applicants and Principal Knowledge Users of Diabetes Action Canada SPOR Network and invited subject matter experts who are responsible for the implementation of all of the programs and projects constituting this research, knowledge translation and training alliance. This meeting is held monthly and is meant to ensure continual communication, relationship-building, collaboration and synergy among our key leaders. The POR Program Committee is an integral part of the Diabetes Action Canada governance structure and provides strategic, critical and innovative thinking in the implementation of Diabetes Action Canada programs and projects.
To see more on this committee click here
[/bs_citem]
[bs_citem title=”
6. Patient Circles
” id=”citem_0d04-7067″ parent=”collapse_dc4e-a604″]
Diabetes Action Canada Patient Circles: Overview and Terms of Reference
Goals of the Patient Circles
The goals of the Patient Circles are:
- to foster patient-oriented research relevant to diabetes; and
- to contribute to better quality research on diabetes and its related complications.
To accomplish these goals, the Patient Circles aim to:
- Bring together diverse groups of people who bring a variety of backgrounds, expertise, ideas, types of diabetes, and personalities
- Foster understanding across these groups
- Create a community of people living with diabetes and their caregivers (hence referred to as Patient partners) who will be involved fully as partners of the Network
- Build capacity for patient engagement in research on diabetes and its related complications in collaboration with the Training and Mentoring Group of the Network
- Ensure that Patient partners are involved at every level (governance, tactical and operational) of the Network and in all phases of the research process (planning of studies, conducting the studies, disseminating the studies’ results, and implementing results of studies)
- Foster communication among and between researchers and those whose lives are most affected by research findings, namely, patients and their family members.
We will regularly report on our progress on these points.
Responsibilities of Members of Patient Circles
- Articulate what matters to patients, families, and communities to inform what diabetes-related research should be done and how it should be done
- Bring knowledge and ways of knowing from other communities to diabetes research
- Support a strong patient voice in working groups, committees and research teams
- Identify and establish local connections to build Diabetes Action Canada’s network of Patient partners
- Share news about Diabetes Action Canada with their communities
- Help disseminate research findings within communities of people affected by diabetes (including, if desired, helping to organize meetings where researchers can bring research findings to communities or health professionals such as certified diabetes educators or dietitians can present best practices)
- Solicit feedback from members of those communities of people affected by diabetes
The Patient Circles adhere to the Guiding Principles set out by the Canadian Institutes of Health Research (CIHR) in the Patient Engagement Framework. These are:
- Inclusiveness: Patient engagement fully integrates a diversity of patient perspectives
- Support: Adequate support and flexibility are provided to patient participation to ensure that they can contribute fully to discussions and negotiations
- Mutual Respect: Researchers, practitioners, and patients acknowledge and value each other’s expertise and experiential knowledge
- Co-Build: Patients, researchers, and practitioners work together from the beginning to identify problems and gaps, set priorities and work together to produce and implement solutions.
This is a living document, as the Patient Circles become more established and as Diabetes Action Canada progresses, changes may be required.
Leadership & Membership of the Patient Circles
To begin, there will be three distinct Patient Circles composed of diverse groups of people who live in Canada and who have diabetes themselves (type 1, type 2 or other types) or who are primary caregivers for persons with diabetes. Each Circle (Collective Patient Circle, Indigenous Patient Circle, Francophone Patient Circle) will include about 12-16 members. The Collective Patient Circle will include at least two liaisons from each of the other Circles. Liaisons will help facilitate smooth communication between Circles and to help ensure that the Collective Patient Circle appropriately incorporates the voices of members of specific populations. Over time, the structures of Circles may change. For example, we initially envisioned having a separate Circle of people who immigrated to Canada as adults, but members of this Circle preferred to be integrated into either the Collective or Francophone Circle, depending on preferred language. We may also add more Circles; for example, we envision possibly adding a French-speaking Indigenous Patient Circle, a Youth Circle, and perhaps others. The Circles will be structured as follows:
Collective Patient Circle
- 12-16 members, at least 4 who are also members of the other 2 Patient Circles
- Persons ensuring functioning of Circle: Holly Witteman, Olivia Drescher
- Additional support: Jon McGavock, Joyce Dogba, Marie-Claude Tremblay
- Anticipated frequency of meetings: 8 meetings per year, 90-minute teleconferences
- Language of meetings: English
Francophone Patient Circle
- 12-16 members, including at least 2 who are also members of the Collective Patient Circle
- Persons ensuring functioning of Circle: Joyce Dogba, Olivia Drescher
- Additional support: Jon McGavock, Holly Witteman, Marie-Claude Tremblay
- Anticipated frequency of meetings: 4 meetings per year
- Language of meetings: French
Indigenous Patient Circle
- 12-16 members, including at least 2 who are also members of the Collective Patient Circle
- Ideally, this Circle will include 2-3 elders
- Persons ensuring functioning of Circle: Alex McComber, Jon McGavock, Marie-Claude Tremblay, Pusha Sadi
- Additional support: Holly Witteman, Joyce Dogba, Olivia Drescher
- Anticipated frequency of meetings: 4 meetings per year
- Language of meetings: Mostly English; Indigenous languages when possible
Patient Circles’ representativeness
Each Patient Circle will aim to have an approximately equal representation of men and women.
Taken together, the Patient Circles will also aim to represent:
- People of different ages, racial, ethnic, and socioeconomic backgrounds.
- People whose lives are affected by type 1, type 2, and other types of diabetes.
- People from different regions of Canada.
- People who are Indigenous from nations located within Canada, settlers born in Canada or who immigrated as children, and people who immigrated to Canada as adults
SPOR Diabetes Network Patient Engagement and Indigenous Health Team Roles
Diabetes Action Canada’s Patient Engagement and Indigenous Health teams will support and coordinate activities of the Patient Circles. They will:
- help plan the meetings;
- organize teleconferences;
- distribute materials and minutes to Patient partners, specifically:
- send meeting documents by email as soon as they are available, in both Microsoft Word and pdf formats, and
- aim to send a final package of meeting documents one week in advance of the meeting, noting documents that are duplicates of those previously sent; and
- Provide administrative and other aid as required by members of the Patient Circle.
Communication guidelines
Our goal in all communication is to understand and be understood. To that end, we will:
- avoid jargon and acronyms as much as possible,
- explain specialized terms whenever it is not possible to avoid using them, and
- Avoid tables and figures in documents to allow screen readers to more easily interpret the document.
Role of the Patient Circles
The Patient Circles are advisory and guidance bodies. They advise and guide Diabetes Action Canada on multiple levels to ensure that the network is responsive to what matters to patients. The Patient Circles advise the Steering Committee. The Steering Committee holds the ultimate governance responsibility for Diabetes Action Canada and has 50% patient or patient representative membership (6 members). Some of these may be members of the Patient Circles.
The Patient Circles also advise on research projects in a number of different ways. Advising on research projects includes discussing research projects at Patient Circle meetings to provide guidance to researchers to help make the research more relevant to patients. Members of Patient Circles as well as other patient members of DAC may also serve as Patient partners on research projects, bringing their expertise from their lived experience with diabetes to the research. Patients can provide expertise in many ways, including their experience of living with diabetes and, if applicable, complications; experience with the health system (care delivery), experience with specific treatments (drugs, surgeries, devices), and community needs.
Levels of Involvement & Time Commitments
All levels of participation are encouraged and welcomed in the Patient Circles. It is understood that the level of involvement and the time commitment possible will vary between members, given the diversity among the Patient Circles members’ jobs, personal commitments, wellness and illness, and other supports. Depending on the level of involvement, the anticipated workload for most Patient partners will be 0.5-2 hours per week.
Members have the option to scale their commitment at any time: When a Patient partner decides to change his/ her level of commitment, he/ she may inform the lead(s) of the research team(s) or Patient Circle(s) and the Patient Engagement Coordinator. Sometimes during times of difficulty in a person’s life, it may be necessary for him/her to step away from his/her role on the Circle. In such cases, the Circle may “keep the person’s seat warm” so that they may return to the Circle when they are able. The Patient Circles will make sure that there is a succession plan for members for when they leave the Circle.
Learning from each other: When new Patient Circle members come on board, they will be offered a brief orientation and mentorship from another member. All Patient Circle members are strongly encouraged to participate in a free training session on Patient-Oriented Research. When a Patient Circle member leaves, the Patient Engagement team will organize a final meeting in which that member may provide any parting thoughts and advice they have to improve our work in future.
Meeting frequency: The Collective Patient Circle will meet approximately eight (8) times per year, for 90 minutes by teleconference, online technology or other method selected by the group. Other Patient Circles will meet approximately four (4) times per year, for 60-90 minutes by teleconference, online technology, or other method selected by the group. These meetings will take place during the time of day or evening most convenient for all participants, alternating if necessary to balance needs. Full-day, in-person meetings will take place at least once per year, budget permitting, ideally in different locations. Meeting frequency and method may be adapted according to the views of Circle members. For example, a Circle may choose to have less frequent, in-person meetings.
Term length: Patient Circle members will initially be encouraged to sit for a term of 1 year, starting from the first full meeting of Diabetes Action Canada Patient Circles, May 2017. After the first year, we hope to maintain at least two thirds of Patient Circle members as active Circle members, with new members joining to help provide new perspectives and allow exiting members to pursue other activities, including possibly other roles within Diabetes Action Canada. Ultimately, we aim to have Patient Circle members take up 3-year terms, with one third of the members finishing their term each year. In this way, participation renewal will be staggered to ensure that there are experienced members, as well as new members on the Patient Circle at all times. Existing members will help informally mentor new members. As the Patient Circles take shape in the first two years, the Patient Engagement team will help to identify which members wish to continue their terms or step back, and will structure ongoing terms accordingly to balance the Circles.
Chairs: Chairship of meetings will be determined by each Circle. It is suggested that chair responsibilities be assumed by those who wish to assume them, sharing responsibilities as needed, with rotating chairs if desired. Meeting chairs will have support from the Patient Engagement team.
Decisions and Quorum: As primarily advisory bodies, Patient Circles will not need to take formal votes frequently. When decisions are required, the Circles will aim for consensus, with an ethic of collaboration, cooperation, and trust, aiming always for respectful debate in which we all seek to understand and be understood. If consensus cannot be reached, those who disagree with the group’s decision may include their concerns in the final report to ensure that these are documented. Because the liaisons represent specific groups who may have particular needs, when decisions are made on the Collective Patient Circle that require a vote, liaisons will be invited to bring issues and/or proposed decisions to their Circles for further discussion prior to the Collective Patient Circle’s vote. The quorum of the Collective Patient Circle (number of members whose presence is necessary to make a binding decision) will be half of its members plus 1, with at least 1 liaison from each other Circle present.
Communication: The Patient Circles will explore options (i.e., methods and frequency) for communication between meetings of the Patient Circles. This can take the form of social media, e-mails, newsletters etc. as deemed most appropriate and effective by the members of the Patient Circles.
Working groups and committees: As the initiative evolves, a number of working groups or standing committees may be established which will provide more focused work. Members of the Patient Circles will be encouraged to join as many working groups as time and interest allows.
Compensation: In recognition for their time spent and valuable expertise, members of the Patient Circles will be offered compensation in accordance with the Diabetes Action Canada Compensation Policy. Compensation will be provided for selected activities, including both meetings and preparation time for meetings. Travel and accommodation costs will be reimbursed. Patient partners will have the option to decline to be compensated.
Opportunity for community at large to provide input to the Circles: Members of the Patient Circles will be ambassadors and champions by liaising with other community organizations and groups. They will bring back any relevant input to the Patient Circles. Members of the Patient Circles are welcome to bring in any idea and/or suggestion from the community for discussion within the Circles.
References
This document draws from a number of other documents, including the Canadian Institutes of Health Research (CIHR) Patient Engagement Framework and the Patient Council Terms of Reference developed by the Can-SOLVE CKD SPOR Network and generously shared with other SPOR Networks.
[/bs_citem]
[bs_citem title=”
7. Project Coordinators Committee
” id=”citem_ee7c-7c89″ parent=”collapse_dc4e-a604″]
The Project Coordinators Committee provides a valuable source of information to the network. They are often the implementers of research and main connection among Goal Groups. They also report on the status of the Research programs and Research enabling programs including activities, progress, deliverables, events, etc.
The Committee comprises the Project Coordinators of the Goal Groups and the staff of DAC Administration. The members of the Committee are:
Chair: Tracy McQuire, Manager/Research Operations & Project Coordinator, Clinical Trials
Members:
- Olivera Sutakovic, Project Coordinator, Diabetic Retinopathy
- Helena Medeiros, Project Coordinator, Health Informatics
- Pusha Sadi, Project Coordinator, Indigenous Peoples’ Health
- Olivia Drescher, Project Coordinator, Patient Engagement
- Michelle Murray, Project Coordinator, Training & Mentoring
- Annie Barbeau Project Coordinator, Knowledge Translation
- Conrad Pow, Project Coordinator, Digital Health to improve Diabetes Care
- Amy Clare, Project Coordinator, Sex and Gender
- Abdelrahman Zamzam, Project Coordinator, Foot Care and prevention of lower extremity Amputation.
- Mildred Lim, Business Officer
- Jessica Antwi, Administrative Assistant
[/bs_citem]
[bs_citem title=”
8. Health Informatics Working Committee
” id=”citem_600c-0b5e” parent=”collapse_dc4e-a604″]
The Health Informatics Working Committee is an ad-hoc committee established to develop a health technology strategy across the research programs of Diabetes Action Canada.
Members of the Health Informatics Working Committee:
Chair: Catharine Whiteside
Members:
Michael Brent, Joe Cafazzo, Jean-Pierre Després, Neil Drummond, Jean-Francois Ethier, Shivani Goyal, Michelle Greiver, France Légaré, Gary Lewis, Tracy McQuire, Bruce Perkins, Conrad Pow, Matthew Tenant, David Wong
[/bs_citem]
[/bs_collapse]
The Health Researcher’s Toolkit: Why Sex & Gender Matter
Women’s Xchange, Diabetes Action Canada’s Sex and Gender Enabling Research Program, has created an interactive and accessible toolkit comprised of 7 e-learning modules focused on the incorporation of sex and gender in research. Women’s Xchange has developed The Health Researcher’s Toolkit: Why Sex and Gender Matter to be as comprehensive as possible, addressing a variety of research methodologies. Sex and gender can be effectively integrated into all research design by asking specific gender questions on questionnaires, disaggregating data by sex or taking a mixed-methods approach – these modules provide a diverse array of strategies to optimize your research in order to become more inclusive.
The modules were reviewed by Diabetes Action Canada’s Patient Partner group and feature the stories of two Diabetes Action Canada Patient Partners. They highlight the importance of Diabetes Action Canada’s Patient Circles and how this model can be used by other researchers to engage with vulnerable groups and populations. The Health Researcher’s Toolkit: Why Sex and Gender Matter provide Diabetes Action Canada research teams with the practical knowledge they need to further enhance the quality of their work.
To access these the Health Researcher’s Toolkit please visit the Women’s Xchange website here
Announcing the Recipients of Diabetes Action Canada Awards (2018-2019)
DAC Training and Mentorship Program Mentorship and Internship Awards 2018-2019
This year, the Diabetes Action Canada Training and Mentoring Program, in collaboration with the Cardiometabolic Health, Diabetes and Obesity Research Network (CMDO), will fund six awards: three Mentorship Awards of $10,000 for a period of one year and three Internship Awards of $10,000 for a period of one year.
We are pleased to announce the successful recipients of the 2018-19 Patient-Oriented Research Early Career Investigator Mentorship Awards and the Patient-Oriented Research Intercentre Trainee Internship Awards and their affiliations:
Mentorship Awardees
1- Anne-Sophie Brazeau – School of Human Nutrition, McGill University
2- Jean-Sébastien Paquette – Département de médecine familiale et de médecine d’urgence, Faculté
de médecine, Université Laval
3- Neeru Gupta – Department of Sociology, University of New Brunswick
Internship Awardees
1- Aleksandra Stanimirovic – THETA Collaborative, Toronto General Research Institute, University
Health Network
2- Dave Bergeron – Faculté de médecine et des sciences de la santé, Université de Sherbrooke et
Faculté de médecine, Université Laval
3- Delnaz Roshandel – The Hospital for Sick Children, Dalla Lana School of Public Health, University of
Toronto
Congratulations and good luck to all the Diabetes Action Canada 2018-2019 Awardees!
New Video: Insights from a Caregiver Research Partner
As posted on the Aging Community Health Website
If you’re a researcher who wants to make the most of the contributions from caregiver partners, you’ll want to watch our latest video.
Gail juggles the demands of being a family caregiver and yet still makes time to be an Aging, Community and Health Research Unit caregiver research partner. In this short video she shares her experience and perspectives about caregiving and sheds light on what researchers really need to know when working with caregivers as research partners. Listen as she reveals what has worked well in partnering with research teams and the benefits she sees of being a caregiver research partner.
Click here to view this video
Click here to view our other videos
Diabetes 360: Framework for a National Diabetes Strategy
As posted on the Diabetes Canada Website
Diabetes Canada released the report “Diabetes 360˚: A Framework for a Diabetes Strategy for Canada. The report contains the recommendations of a coalition of nearly 120 experts from across Canada.
CMAJ – A home for patient-oriented research
CMAJ has recently announced CMAJ Open Patient-Oriented Research Collection.
This is an exciting opportunity for patient-oriented researchers as it provides a home for research studies that particularly specify how patients were engaged as part of the research team and how their contributions developed the work. This group is guided by a steering committee composed of researchers and patients from across Canada and each article considered for the collection will be reviewed by both patient and peer reviewers.
Patient-Oriented research is still an emerging concept that takes time to accumulate an evidence base and to build enough collective knowledge to shape methodology. By creating a dedicated open-access repository for rigorous patient-oriented research, CMAJ Open hopes to provide a platform to answer questions about how best to engage patient partners and evaluate their impact on health research. This will inform best practice and ultimately put relevant knowledge that matters into the hands of both patients and health professionals who can use it to improve health outcomes.
Already a podcast has been released by CMAJ as part of the Patient-Oriented Collection
Author guidelines for this collection are available as well as guidelines for patient peer reviewers.
If you or someone you know would be willing to review papers for the POR collection, it is a matter of clicking here to ‘Create an Account’, then adding “Patient Oriented Research” to areas of expertise when prompted. If you are as Patient Partner also add “Patient Reviewer” under areas of expertise.
If you have any questions about eligibility and guidelines, please direct them to CMAJ at editorial-open@cmaj.ca.
Community Voices: Diabetes in Indigenous Populations
Community Voices: Diabetes in Indigenous Populations is a video project produced by the Institute of Health Economics in Alberta Canada and support by Boehringer-Ingelheim Canada. This video aims to highlight Indigenous perspectives on health, and promote shared learning for a variety of stakeholders within the context of health, well-being, and health care in Canada.
New videos from the series will be added regularly to the Institute for Health Economics website here, and will highlight voices from Indigenous communities describing current issues of concern, and aspirations for the future.
Community Voices: Diabetes in Indigenous Populations – Part One
Description
The video above captures voices from the Assembly of First Nations Health Transformation Summit, which took place February 13-14, 2018.
A special thank you to Dr. Angela Mashford Pringle, Assistant Professor, University of Toronto, and Associate Director, Waakebiness-Bryce Institute for Indigenous Health; Carol Hopkins, Executive Director, Thunderbird Partnership Foundation; Regional Chief Isadore Day, Assembly of First Nations; and the Assembly of First Nations for supporting the development of this video.
Background
The Institute of Health Economics hosted a policy roundtable Diabetes Care and Management in Indigenous Populations in Canada in the Fall of 2017. A major theme emerging from the roundtable was the importance of community engagement and leadership in the development of effective health programming, which is a key component of several current initiatives at both local and national levels. At a national level, the Assembly of First Nations Health Transformation Agenda aims to support the development of health systems led, managed, and operated by First Nations communities, for First Nations communities. At the community level, there are several successful diabetes care and management programs, including the Kahnawake Diabetes Prevention Project, Diabetes and My Nation, and the Indigenous Diabetes Health Circle, among many others, which were developed by communities to address self-identified priorities and needs.
Acknowledgements
This project was only possible through the generous contributions of many individuals across Canada, and their willingness to participate and share their perspectives, thoughts, and ideas with us, and to offer their comments and feedback on earlier versions. We thank them for their time, contributions, and seemingly limitless patience teaching us.
Project Sponsor
This project was completed with funding support, and in partnership with Boehringer Ingelheim (Canada) Ltd.
A Common Vision for Increasing Physical Activity and Reducing Sedentary Living in Canada: Let’s Get Moving
On May 31, 2018, federal, provincial and territorial (FPT) governments released A Common Vision for Increasing Physical Activity and Reducing Sedentary Living in Canada: Let’s Get Moving. This is Canada’s first ever national policy focusing on increasing physical activity and reducing sedentary living in Canada.
Led by the Public Health Agency of Canada at the federal level, the purpose of the Common Vision is to guide FPT governments and non-governmental organizations (NGOs) in addressing physical inactivity and sedentary behaviour among Canadians of all ages and abilities across the life stage. It reflects integrated approaches and solutions from across various sectors of society, as all orders of government build on existing efforts in this area, including how governments align and complement efforts with non-governmental organizations to increase physical activity and reduce sedentary behaviour in Canada.
The Common Vision was developed and designed collaboratively by FPT governments and was informed by a comprehensive, Pan-Canadian consultation and engagement process that included focused outreach on specific issues facing municipalities, Indigenous on and off-reserve communities, as well as northern, rural and remote communities.
The Common Vision aligns with, amplifies and supports the goals and objectives of existing policies, strategies and frameworks in Canada.
It was also informed by relevant Calls to Action of the Honouring the Truth, Reconciling for the Future: Summary of the Final Report of the Truth and Reconciliation Commission of Canada (2015).
On a global scale, the Common Vision aligns with and supports the World Health Organization’s Global Action Plan on Physical Activity, which was adopted at the 71st World Health Assembly on May 25, 2018 to encourage a comprehensive and coherent response for global and national action using a collaborative partnership approach.
Learn more about the Common
Vision<https://www.canada.ca/en/public-health/services/publications/healthy-living/lets-get-moving.html>.
_________________________________________________________________
Document Publication Date: 2018-06-01
Document Deletion Date: 2019-05-31
Category: 2. Headline News
Author Branch/Agency: HPCDP
Responsible Organization: Centre for Chronic Disease Prevention Approved By: Barrett Halliday/HC-SC/GC/CA
Contact: Joe Doiron/HC-SC/GC/CA