New research project tests the use of technology to support those with diabetes distress

By Krista Lamb
On March 3rd, Brain Canada and JDRF announced the winners of their Addressing Mental Health in Type 1 Diabetes Team Grants competition. Diabetes Action Canada was thrilled that one of our supported projects was selected.
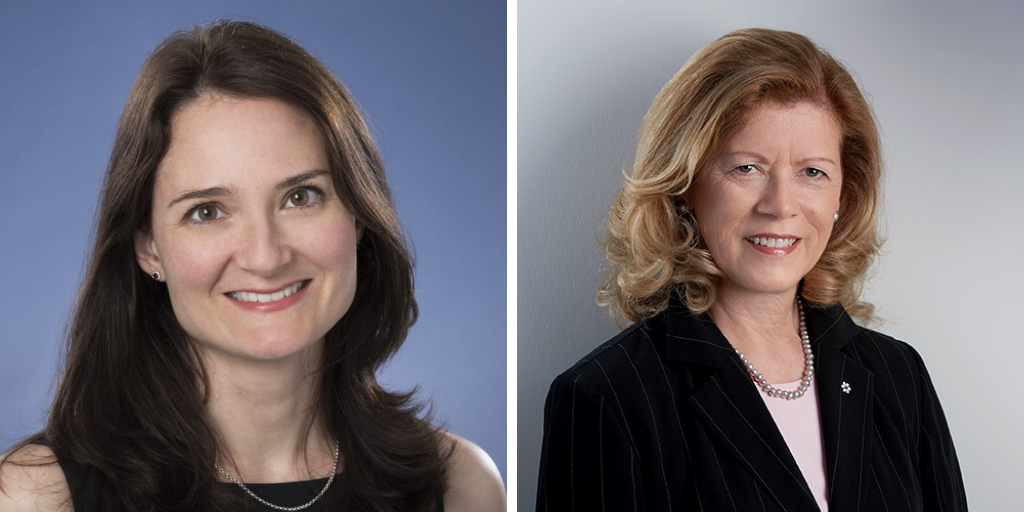
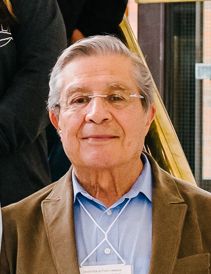
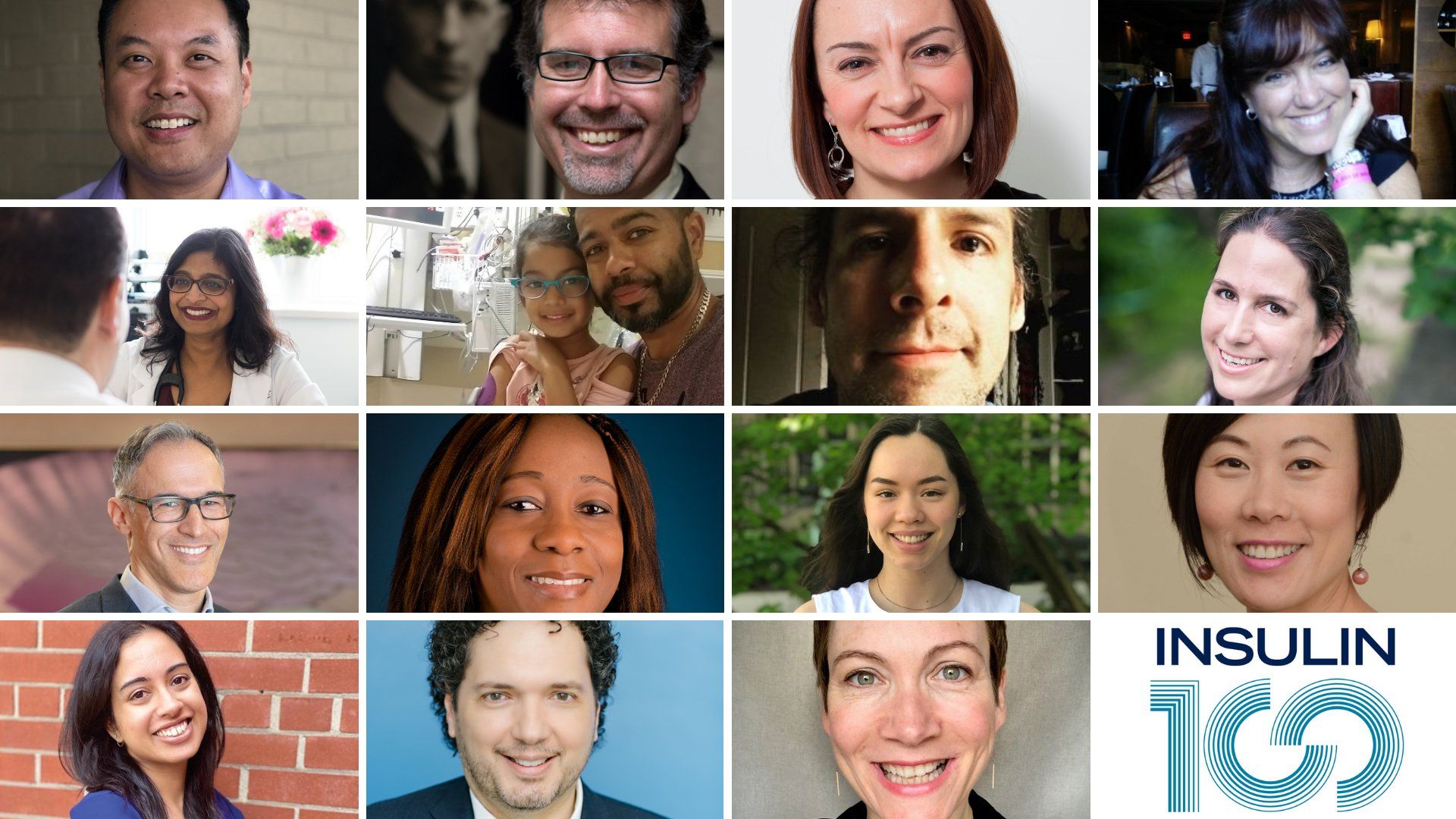
Dr. Peter Selby from the Centre for Addiction and Mental Health (CAMH) will be the lead investigator looking into “Technology-enabled comprehensive care for young adults with type 1 diabetes (T1D) experiencing diabetes distress”. He is joined by co-investigators Drs. David Castle and Gillian Strudwick from CAMH and Dr. Diana Sherifali from McMaster University, who also co-lead the newly established Mental Health and Diabetes research program for DAC, as well as Dr. Bruce Perkins from the Leadership Sinai Centre for Diabetes and Dr. Peter Senior, Director of the Alberta Diabetes Institute, who lead the Innovations in T1D program. Five Diabetes Action Canada Patient Partners helped develop the grant application and they will be at the table throughout the planning for this research proposal.
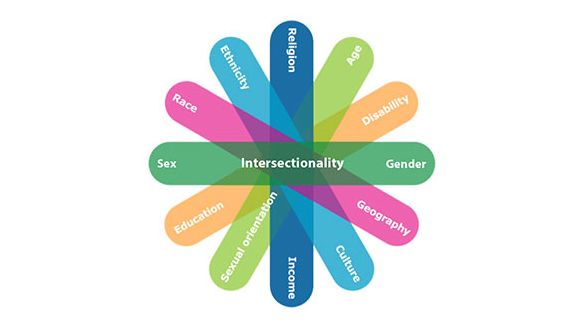
This project looks specifically at co-developing effective supports to help people between 18 – 29 with T1D manage diabetes distress, a condition which affects more than 40% of those living with the condition. Diabetes distress is the emotional burdens and worries that accompanies the need to constantly self-manage diabetes.
“We have heard from people living with diabetes how important and how real diabetes distress is,” says Perkins. “This team is figuring out how to help people identify distress, and how to help deal with it using virtual care. We are confident that this could change the way the health care system actually helps real people with real issues in an efficient way.”
With an increasing number of people using technology to help them manage their diabetes, this project incorporates proven technologies like video chat and text messages to offer mental health support. The program being developed uses techniques from, The Optimal Health Program, which was designed to explore the origin of wellbeing within every person, and to support those who use it to promote self-agency in the face of life’s challenges. With trained mental health and diabetes experts guiding the process, the hope is to safely reduce barriers to needed resources.
“To improve patient-centred approaches, we will be able to co-design and test technology to bridge the gaps in care delivery between the mental health system and diabetes care and empower people to manage their own mind-body wellbeing,” says Selby.
For the Patient Partners involved in the research planning phase, access to appropriate support systems and education about how to find these resources were key priorities. Currently, diabetes-focused mental health interventions are limited, especially outside major city centres. It is also difficult to find health care providers with experience diagnosing or treating diabetes distress. Technology may be able to help by leveraging the available resources and reducing barriers to access, but it can only help if it is designed with the unique needs of people living with diabetes at the forefront.
“I think everyone with T1D struggles at some point with diabetes distress and mental health, but rarely is this raised with health care providers,” says Senior. “It would be easy for researchers to propose a solution based on assumptions or their narrow perspective. However, unless we take the time to hear from people living with diabetes about how they experience the problem and have them direct the design of a solution, there is a huge risk that we will miss the mark.”
The research team also includes Diabetes Action Canada researcher Dr. Joe Cafazzo and the Connect1d Canada team. The project will begin the initial phase of the project this spring.